Soft Tissue & Bone Infections
Skin and soft tissue infections (SSTIs) typically occur when skin flora penetrate underlying layers of the epidermis due to some sort of defect in the skin barrier. Trauma (an abrasion or penetrating wound), onychomycosis, tinea pedis, vascular or lymphatic compromise, and diabetes are common predisposing factors.
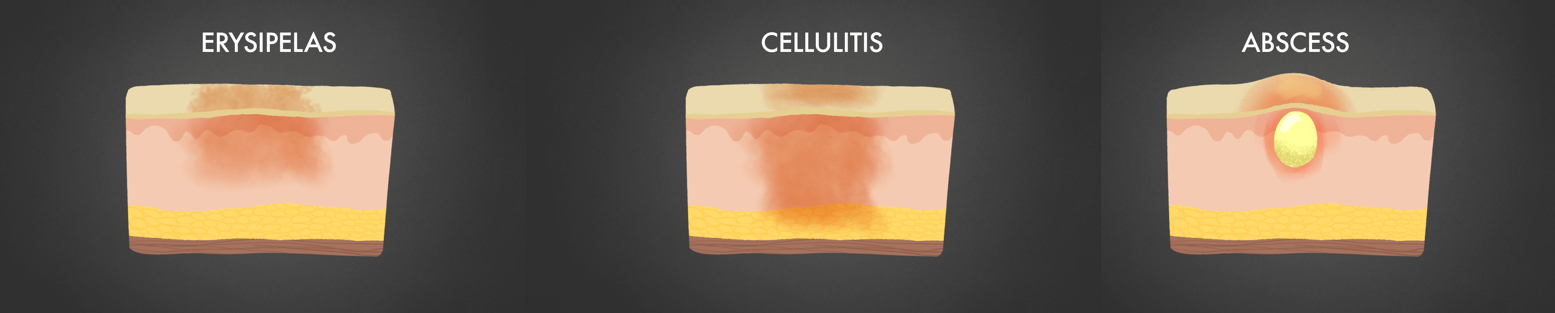
Cellulitis, abscess, or both are the most common SSTIs; cellulitis (which includes erysipelas, a superficial infection that occurs more commonly in children and involves the face or lower extremities) manifests as an area of skin erythema, edema, and warmth. An abscess is a collection of pus within the dermis or subcutaneous space.
(We make pus look cute.)
The most common organisms causing SSTIs are beta-hemolytic streptococci (especially group A strep and group B strep in diabetic patients) and Staph aureus, although there are lots of flavors of cellulitis based on specific exposures! See Table 1 below; the boards often have a question or two on these.
Table 1. Specific cellulitis pathogens based on exposure history:
|
Exposure |
Pathogen |
Comments |
|
Recreational water sports (freshwater or brackish) or leech therapy |
Aeromonas hydrophila |
|
|
Contact with saltwater or brackish water from seafood drippings |
Vibrio vulnificus, other Vibrio spp. |
Can cause cellulitis from skin inoculation OR can be ingested and cause bacteremia with secondary skin infection. Hemorrhagic bullae are classic. Severe infection occurs in patients with iron overload states (cirrhosis, etc.) |
|
Contact with cats |
Pasteurella multocida |
Cellulitis at area of cat scratch or bite |
|
Contact with dogs |
Capnocytophagia canimorsus |
Cellulitis and fulminant sepsis especially in asplenic patients (often fatal!) |
|
Contact with infected animals or animal products, bioterrorism target |
Bacillus anthracis |
Swollen pruritic lesion with central eschar |
|
Contact with or bite from infected mammal (cats, rabbits) or tick bites |
Francisella tularensis |
Ulceroglandular syndrome—ulcer with central eschar and localized LAD |
|
Contact with fresh/salt water, fish tanks and swimming pools |
Mycobacterium marinum |
Usually involves the upper extremities with papular lesions that become ulcerative (can look like Sporothrix due to lymphatic spread!) |
|
Contact with freshwater footbaths (nail salons), after breast augmentation and open heart surgery |
Mycobacterium fortuitum |
Multiple boils, associated with areas of razor shaving |
It’s easiest to group these based on what tissues are involved: Erysipelas is a superficial infection of the epidermis and classically has well-demarcated borders. Cellulitis (which could be purulent or non-purulent) involves the dermis and subcutaneous tissues and has poorly-defined erythema. Cellulitis with purulence is most often due to MRSA, and community-associated MRSA (CA-MRSA) has become the scourge of gyms, athletic teams, military recruits, and correctional facilities… essentially anywhere with crowding, which leads to suboptimal hygiene.
As you’d expect, the diagnosis of SSTIs is made clinically as the causative agent is only found in a few patients (often only when purulent discharge is sent for culture.) Blood cultures are positive in less than 5% of patients. Imaging should only be ordered if you’re uncertain or when you suspect an abscess or necrotizing fasciitis.
Practical Pearl
Bilateral cellulitis?
Cellulitis is often misdiagnosed—clinicians often mistake stasis dermatitis, contact dermatitis, lymphedema and DVT as cellulitis! Remember that a patient being admitted for “bilateral cellulitis” is highly suspicious for a diagnosis other than cellulitis because cellulitis is rarely symmetrical.
Treatment (both inpatient and outpatient) is straightforward:
Cellulitis (no pus): Use cefazolin IV
Cellulitis (with pus): Use vancomycin IV (goal trough 10-15)
If you see an abscess, I&D it (and get a culture if possible)! For abscesses <2 cm in size, I&D without antibiotics is enough. Antibiotics are generally only recommended if there is extensive infection, if I&D is inadequate, in immunocompromised patients, or in difficult-to-drain areas such as the genitalia, hands or face.
Outpatient/oral regimens:
Non-purulent cellulitis (Strep spp.): cephalexin, cefadroxil or dicloxacillin can be used in lieu of cefazolin
Purulent cellulitis (MRSA): TMP-SMX, doxycycline or linezolid may be used in lieu of vancomycin
How about duration? Unfortunately, there is no hard and fast rule for duration of antibiotic therapy for cellulitis—you treat until you achieve clinical resolution, typically on the order of 5-10 days. Some patients may require longer durations (~14 days) if they have extensive infection.



